Psilocybin for Cluster Headaches: Treatment Protocol and Patient Experiences
Introduction
Cluster headaches—often referred to as “suicide headaches”—are among the most debilitating pain conditions in medicine. Affecting approximately 0.1% of the population, these occur in cyclical patterns with multiple daily attacks localized around one eye. Unlike other types of headaches, cluster headaches are shorter in duration but far more intense. Patients often experience weeks- or months-long cycles followed by remission phases.
Traditional treatment options are limited and can be ineffective for many sufferers. Pharmaceutical treatments such as verapamil, lithium, and triptans offer relief for some, but many experience adverse side effects or minimal efficacy. In response, a growing number of patients are exploring alternative therapies—most notably, psilocybin, the psychoactive compound in “magic mushrooms.”
Initially studied for its role in treating depression and PTSD, psilocybin draws interest for its effectiveness in treating cluster headaches, especially in the form of microdosing or periodic, larger doses. Patients report that this approach can prevent attacks or dramatically reduce their severity.
The potential efficacy stems from psilocybin’s interaction with serotonin receptors, particularly 5-HT2A. This receptor is connected to pain modulation, circadian rhythm regulation, and blood vessel constriction—all relevant in the pathology of cluster headaches.
While large-scale clinical trials remain scarce, real-world experiences, smaller studies, and case reports increasingly support psilocybin’s therapeutic potential. This article reviews the scientific understanding, proposed treatment protocols, and first-hand patient experiences.
Scientific Features and Evidence
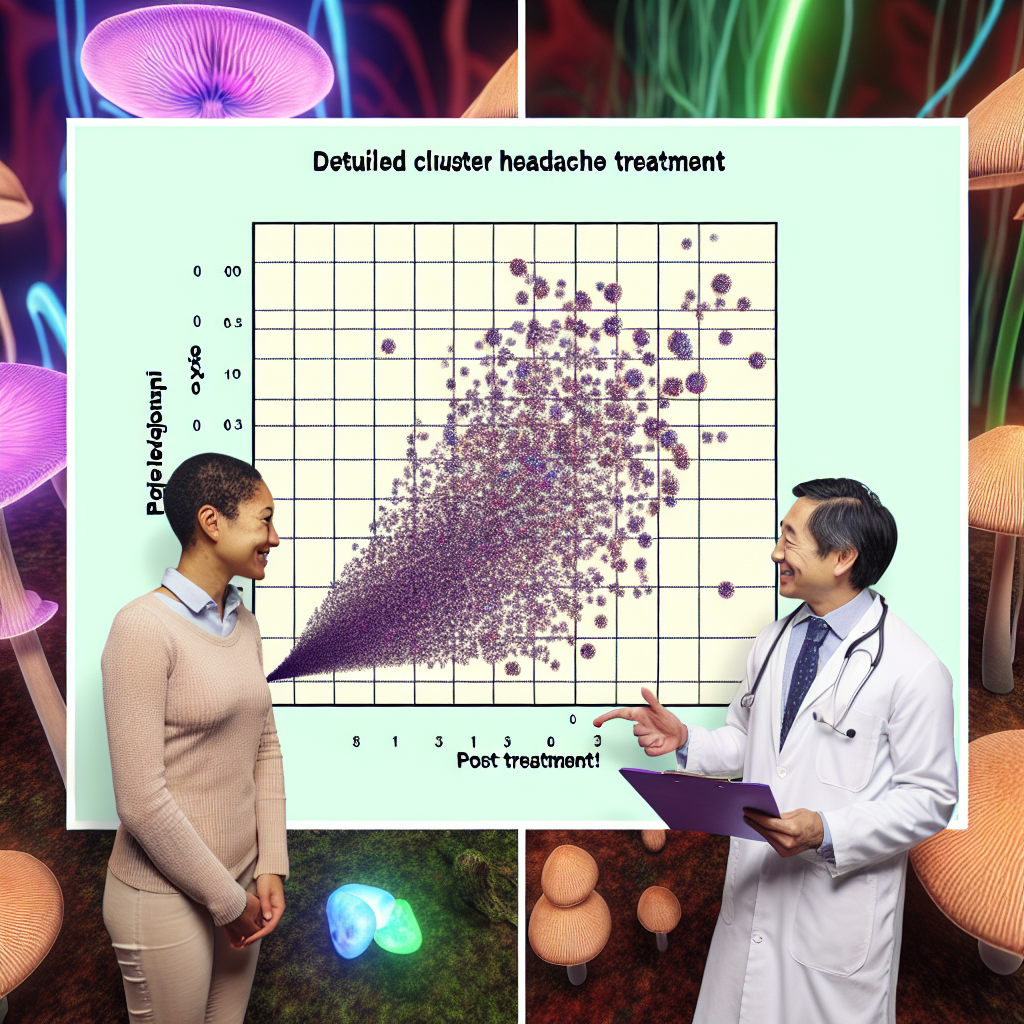
Although still classified as a Schedule I substance in many countries, interest in the therapeutic benefits of psilocybin is surging. A landmark 2006 survey published in the journal Neurology by Dr. Andrew Sewell of Harvard Medical School found that 85% of cluster headache sufferers who tried psilocybin or LSD experienced significant relief—either stopping a current attack or preventing a full-blown cycle.
Further insights from the journal Cephalalgia and other sources indicate that psychedelics may work by affecting the hypothalamus, a brain region involved in both circadian regulation and cluster headache etiology. Through modulation of serotonergic pathways, psilocybin may restore regulation and provide a protective effect against cluster cycles.
The Clusterbusters community, a nonprofit dedicated to alternative treatments for cluster headaches, has contributed citizen science data that supports two common protocols: microdosing (0.1–0.3g every 2–3 days) and “busting” (larger doses at key cycle moments). These protocols are widely shared and responsibly discussed among patient forums.
A commonly referenced dosing procedure, especially for those entering a new cycle, involves three doses spaced five days apart—a protocol designed to both interrupt the cycle and regulate future episodes. Some patients use maintenance microdosing between clusters to extend remission.
Notably, psilocybin appears to be non-addictive and relatively well-tolerated. However, it should be approached cautiously by patients undergoing psychiatric treatment or those using SSRIs, due to potential interactions. Importantly, the U.S. Food and Drug Administration has granted Breakthrough Therapy Designation to psilocybin for depression, signaling heightened interest and future regulatory change.
Patient Experiences and Protocols
Anecdotal evidence from platforms like Clusterbusters.org and Reddit’s ClusterHeads subreddit illustrates the profound effects patients experience with psilocybin therapy.
Jake, a 38-year-old with chronic cluster headaches for over a decade, reports: “No pharmaceutical worked for me. After two busting doses with psilocybin at the start of my usual cycle, the pain vanished. I haven’t had an active period since.”
Maria, who follows a maintenance protocol of 0.15g every three days, hasn’t had a cluster cycle in 18 months. “It feels like I have control over my health again. For once, I’m not living in fear,” she says.
Many patients emphasize the importance of regimen timing. Most agree the protocol is more effective if started at the earliest sign of a cycle. Using psilocybin during an ongoing attack might not always stop the pain immediately but can significantly reduce the duration and severity of subsequent episodes.
Typical regimens include:
– Microdosing: 0.1–0.3g every 2-3 days during remission or leading up to an expected cycle.
– Busting: 0.5–2g doses spaced five days apart at the start of a predicted cluster cycle.
– Maintenance: Continued microdosing during high-risk periods based on individual history.
Users stress quality sourcing, taking psilocybe cubensis, avoiding alcohol, and discontinuing triptans for best results.
Conclusion
The use of psilocybin for cluster headaches offers a powerful example of how natural substances may serve as effective treatments when conventional medicine fails. Despite its legal and regulatory challenges, early research and strong anecdotal evidence support its efficacy and safety as a treatment option.
As more research develops and regulations evolve, psilocybin could transition from an underground remedy to a legitimate, well-studied alternative for those living with chronic cluster headaches. For many, it represents much more than symptom relief—it provides hope, autonomy, and the freedom to live without debilitating pain.
Concise Summary
Psilocybin, the active compound in magic mushrooms, is gaining attention as an effective alternative treatment for cluster headaches. Sufferers report that both microdosing and larger “busting” doses prevent or drastically reduce cycles, often when conventional medications fail. Scientific studies suggest that psilocybin’s action on serotonin receptors and the hypothalamus may underlie these effects. Although clinical trials are limited, growing user communities and evidence support its promise. With careful dosing protocols and legal awareness, psilocybin could revolutionize how cluster headaches are managed and offer renewed quality of life.
References
– Sewell, R. Andrew, Halpern, John H., and Pope Jr, Harrison G. “Response of cluster headache to psilocybin and LSD.” Neurology, 2006
– Kometer, M., and Vollenweider, F.X. “Serotonergic hallucinogen-induced visual perception: a review of functional neuroimaging studies.” Current Topics in Behavioral Neurosciences, 2016
– Clusterbusters: https://clusterbusters.org
– FDA Breakthrough Therapy Designation for Psilocybin: FDA.gov

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives. Film Student and Full-time Medical Writer for ContentVendor.com