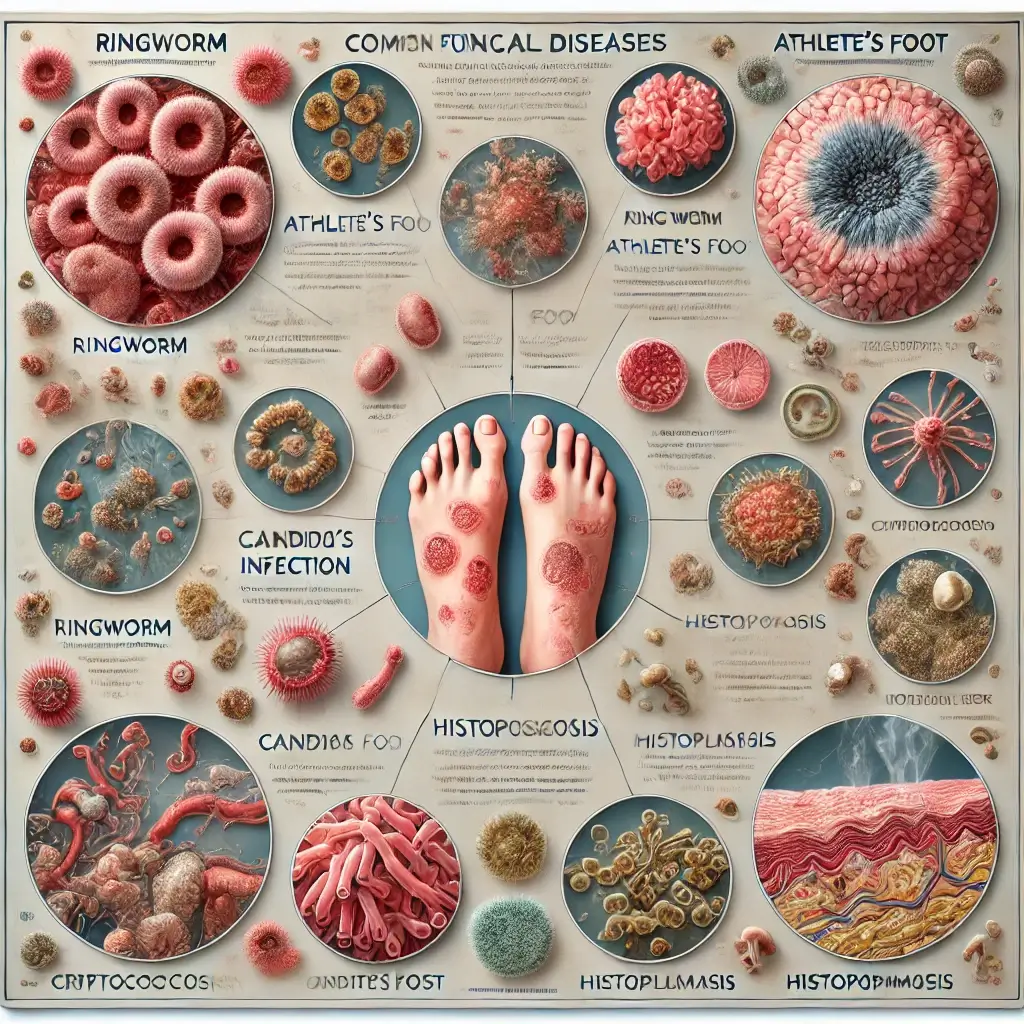
Understanding the Diversity of Fungal Pathogens
Fungi encompass a wide array of organisms that has the capability to induce diseases in human beings. Fungal illnesses exhibit a spectrum of severity, encompassing both mild and severe manifestations, and possess the capability to impact several anatomical regions inside the human body.
Common Fungal Infections You Should Know
Several fungal infections are often observed, including:
Ringworm, also known as dermatophytosis, is a prevalent fungal illness characterized by the appearance of a circular, erythematous rash. The condition has the potential to impact the integumentary system, specifically the skin, scalp, and nails.
Athlete’s foot, also known as tinea pedis, is a dermatophytic fungal infection characterized by pruritus, erythema, and desquamation of the interdigital spaces.
Candida, scientifically known as Candida spp., is a genus of yeast that has the potential to induce a range of illnesses, encompassing vaginal candidiasis, diaper dermatitis, and oral candidiasis.
Cryptococcosis, a fungal infection, has the potential to impact many organs such as the lungs, brain, and other bodily systems. Prevalence of this condition is highest in those with compromised immune systems.
Histoplasmosis is a fungal illness resulting from the inhalation of spores originating from avian or chiropteran excrement. It has the potential to induce symptoms that resemble those of pneumonia.
Risk Factors Behind Fungal Infections
Fungal illnesses can arise due to a multitude of reasons, encompassing:
Fungal exposure: Fungi are ubiquitously present in several environmental reservoirs, including soil, water, and plant surfaces. The likelihood of contracting a fungal infection can be elevated via exposure to fungus.
Individuals with compromised immune systems, such as those afflicted with HIV/AIDS or cancer, have an increased susceptibility to the development of fungal infections.
Certain underlying medical disorders, such as diabetes and renal illness, have been found to elevate the susceptibility to fungal infections.
Specific medications: Certain pharmaceutical drugs, such as corticosteroids and antimicrobial agents, have the potential to compromise the immune system’s functionality, hence augmenting the susceptibility to fungal infections.
Recognizing the Warning Signs of Fungal Disease
The manifestation of symptoms associated with fungal diseases exhibits variability contingent upon the specific kind of infection. Several often observed symptoms include:
The presence of a circular, erythematous rash is a frequently observed manifestation of ringworm infection.
Pruritus: Pruritus is a prevalent manifestation associated with several fungal diseases.
Burning sensation is a prevalent manifestation associated with athlete’s foot.
The manifestation of scaling on the skin is a prevalent clinical indication observed in cases of athlete’s foot and ringworm.
Open wounds may indicate the presence of a potentially severe fungal infection, such as cryptococcosis.
Chest discomfort may serve as an indicator of a potentially severe fungal infection, such as histoplasmosis.
Treatment Options for Fungal Infections
Seeking medical attention from a healthcare professional is crucial if one suspects the presence of a fungal infection, as it facilitates accurate diagnosis and appropriate therapeutic intervention. The choice of treatment for fungal illness is contingent upon the specific type of infection. Several commonly used therapies include:
Antifungal medication: Administration of antifungal drugs can be achieved either oral ingestion or topical application into the skin.
Surgical intervention may be deemed required in cases when a fungal infection has disseminated to the skeletal structure or other bodily organs, warranting the removal thereof.
Supportive treatment, which encompasses interventions such as administration of fluids and medicines, may be deemed essential in the management of a severe fungal infection.
The Prognosis and Importance of Early Treatment
Fungal illnesses has the potential to induce significant morbidity, however they frequently exhibit amenability to therapeutic interventions. Seeking medical attention from a healthcare professional is imperative when suspecting the presence of a fungal infection, as it allows for accurate diagnosis and appropriate therapeutic intervention.
Preventive Strategies Against Fungal Diseases
Listed below are many recommendations aimed at mitigating the occurrence of fungal infections:
It is advisable to maintain cleanliness and dryness of the skin. This intervention will aid in inhibiting the proliferation of fungal organisms.
It is advisable to refrain from coming into touch with dirt, soil, as well as bird or bat excrement. These substances have the potential to harbor pathogenic fungus that can lead to infection.
It is advisable to use footwear when traversing public areas without any covering on the feet. This measure will aid in safeguarding one’s foot against fungal infections.
It is advisable to maintain cleanliness and proper grooming of one’s nails. This measure will aid in the prevention of fungal development beneath the nails.
It is important to manage and attend to one’s diabetic condition. Diabetes mellitus has been found to have a detrimental effect on the immune system, hence elevating the susceptibility to fungal infections.
It is advisable to adhere to the prescribed prescriptions provided by one’s healthcare professional. This intervention aims to address any preexisting medical issues that might potentially heighten the susceptibility to fungal infections.
By adhering to these guidelines, individuals can effectively mitigate the risk of contracting fungal infections and maintain optimal health.
References
- Centers for Disease Control and Prevention. (2023). Fungal Diseases. Retrieved from https://www.cdc.gov/fungal/
- World Health Organization. (2022). Fungal Infections. Retrieved from https://www.who.int/health-topics/fungal-infections
- Bongomin, F., Gago, S., Oladele, R. O., & Denning, D. W. (2017). Global and Multi-National Prevalence of Fungal Diseases—Estimate Precision. Journal of Fungi, 3(4), 57.
- Pappas, P. G., Lionakis, M. S., Arendrup, M. C., Ostrosky-Zeichner, L., & Kullberg, B. J. (2018). Invasive candidiasis. Nature Reviews Disease Primers, 4, 18026.
- Perfect, J. R. (2019). The impact of the host on fungal infections. American Journal of Medicine, 132(12), 1379-1386.